UPDATED: 10/25/2018
“Nobody really knows what causes Crohn’s Disease; the first person to figure that out will probably win the Nobel Prize,” says Granite Peaks Gastroenterologist Andrew Heiner, MD.
Dr. Heiner, who diagnoses and treats many patients with Crohn’s each year, is incredibly hopeful that in the next several years, the mystery behind the cause of the disease will be solved. In the meantime, he points out that advancements in medication in the last decade have allowed most people with the disease to regain their health and quality of life.
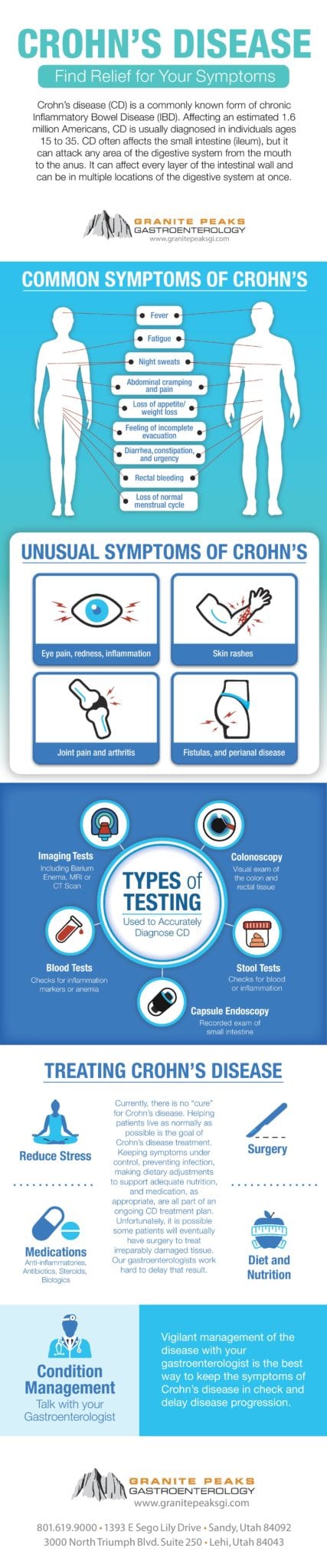
Named after Dr. Burrill Crohn, who first described the disease in 1932 along with two other colleagues, this life-long disease is a specific type of Inflammatory Bowel Disease (IBD). Crohn’s Disease can affect any part of the gastrointestinal tract; it most commonly affects the end of the small bowel (the ileum) and the beginning of the colon. Often it is confused with ulcerative colitis, another type of IBD that exclusively affects the large intestine (colon).
Some 700,000 Americans, men and women equally, live with Crohn’s Disease, many of whom were diagnosed between the ages of 15 and 35. While the disease is usually diagnosed in people who are in their teens and early twenties, it is not uncommon to see it surface in the 50-70 year-old-age range as well. Patients most often come in complaining of abdominal pain – a result of small intestinal inflammation. Diarrhea and bloody stools are common symptoms if the inflammation is in the colon. “Some patients have inflammation in both areas and are completely miserable while others have minimal symptoms and we would never know they have Crohn’s without doing more testing,” says Dr. Heiner. He also points out that patients may have non-intestinal manifestations like fatigue, arthritis, swollen, blood shot eyes, and rashes.
“The pain can be intense and it is not an uncommon scenario for patients to be diagnosed with appendicitis and end up in surgery only to discover that they actually have Crohn’s,” adds Dr. Heiner.
While Crohn’s is a life-long disease, it can sometimes go into remission for years. “We never consider anyone to be cured. Most people will eventually end up back at the doctor’s office if they are not on treatment,” says Dr. Heiner, adding that while the environmental triggers are different for everyone, smoking is without a doubt one of the most exacerbating factors. Emotional stress, physical stress, lack of sleep, dietary changes or pregnancy may all trigger flare-ups – although some women actually improve while pregnant. “It is a very unpredictable disease and affects each person differently, making it challenging to treat, but also rewarding because each patient is unique and you get to know them well,” says Dr. Heiner, who has seen some of his patients with Crohn’s for more than 25 years.
Genetics is also a factor. Some 5 to 20 percent of affected individuals have a first-degree relative (i.e., a parent, child, sibling) with the disease. The risk is also substantially higher when both parents have IBD. While the disease is most prevalent among eastern European backgrounds, an increasing number of cases are being reported among the African-American population.
“It used to be so frustrating years ago to see how miserable these patients were and all we could offer them were steroids that came with all sorts of complications,” recalls Dr. Heiner. Now, medications have evolved and diversified, allowing for treatment using oral anti-inflammatory medications and steroids, immune-suppressants, and for more severe cases, biologics (a genetically engineered therapy made from living organisms) and biosimilars. There are even more options in the pipeline. “I’ve gone from the frustration of not being able to help certain patients with severe disease, to being able to help most patients live a normal, healthy life,” adds Dr. Heiner.
The earlier the treatment, the better for the patient. Early detection is key in treating Crohn’s; the sooner it is diagnosed the easier it is to treat and the better the patient will do long term. Surgery may be required but patients still have better outcomes when they have surgery as soon as it is needed vs waiting. Surgery is necessary when inflammation has created thickening of the intestinal wall, constricting it to a point that it doesn’t allow a passageway, which can be deadly. “Sometimes after surgery, the Crohn’s can return at the site of the surgery, so we first and foremost prefer treating patients aggressively with the appropriate medications,” says Dr. Heiner.
Dr. Heiner recalls one of his patients, a young man earning his master’s degree, who had one of the most severe cases of Crohn’s he had yet seen. The inflammation involved his stomach all the way down to his small intestine. In intense pain and having lost more than 35 lbs., the young man was beside himself, not knowing what was going on. Dr. Heiner immediately put his new patient on biologic injections and two to three weeks later, this young man was back to living a normal graduate student’s life. He was able to complete his education and is free of stomach problems. Dr. Heiner affirms, “Witnessing this kind of complete turnaround in quality of life is the most rewarding aspect about treating my patients with inflammatory bowel disease.”
To schedule an appointment at Granite Peaks Gastroenterology with one of our board-certified gastroenterologists, click here. You don’t need a physician referral and nearly all insurances are accepted. Granite Peaks can usually see patients within one week for office consultations and/or procedures, or sooner if the need is emergent.
Call (801) 619-9000 with any additional questions. Granite Peaks has offices in Sandy and Lehi and procedures are performed at our Endoscopy Center in Sandy.